September 7, 2024
Urinary System Incontinence In Females: Kinds, Therapies, And Expectation
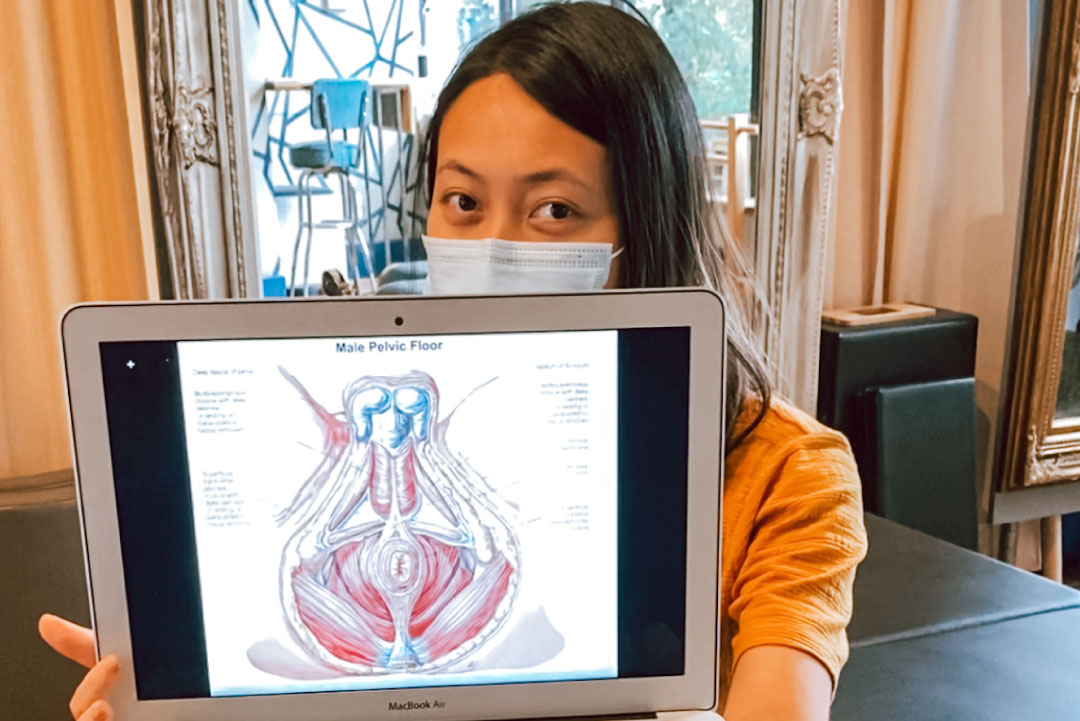
Remedies For Your Urinary System Incontinence: Melissa Grier, Md: Obgyn Pelvic flooring weakening is a significant contributor to urinary system incontinence throughout menopause. The pelvic floor muscular tissues, which support the bladder and urethra, can come to be extended and deteriorated because of hormone changes, giving birth, and aging. This weakening can cause a loss of bladder control, causing urinary system incontinence. Furthermore, variables such as weight problems and chronic coughing can additionally stress these muscle mass, exacerbating the issue. Ladies might additionally experience a decline in muscle mass coordination, making it difficult to engage the pelvic flooring muscular tissues successfully when needed, which can bring about enhanced episodes of leak. The strongest evidence of advantage is for overseen PFMT in women with tension urinary incontinence, with less efficiency in those with seriousness incontinence111.Blended Incontinence Diagnosis
Encouraging women with knowledge concerning treatment options, dealing methods, and preventive measures can aid them handle urinary system incontinence properly and live with confidence. Reduced estrogen levels during menopause can weaken the pelvic flooring muscular tissues and the urethral sphincter, contributing to urinary incontinence. The American College of Obstetricians and Gynecologists (ACOG) mentions that normal exercise and preserving a healthy weight are vital consider avoiding UI and improving bladder control. The ACOG also advises pelvic flooring muscle exercises, additionally referred to as Kegel workouts, to reinforce the muscular tissues that sustain the bladder.Discover A Therapy Facility
Symptoms typically include constant peeing, nocturia (waking in the evening to urinate), and the failure to manage the urge to pee. The bladder, urethra and urinary system sphincters work in show to store pee at reduced stress and to invalidate voluntarily at socially practical or proper times. The detrusor muscular tissue and inner urethral sphincter are primarily smooth muscle, whereas the outside urethral sphincter and pelvic floor muscle mass are mainly striated muscle mass. You can take a trip and take part in physical activities with menopause-related urinary incontinence. Methods like practicing desire reductions and making use of urinary incontinence products can aid manage leak throughout travel. Regular exercise, specifically low-impact exercises that reinforce the pelvic floor, can aid enhance bladder control. Only do this up until you find out how to find the muscular tissues-- quiting the flow of urine mid-stream isn't healthy and balanced over a long website period of time. Urinary system incontinence is a common condition impacting several individuals, especially postmenopausal females. Hormonal agent substitute therapy can help alleviate this ailment, mostly through estrogen supplements to help revive the vitality of your reproductive tract. Nevertheless, this therapy has several threats, and you should just do it after consulting with your medical professional to know what is finest for your unique instance. If you have extra questions concerning the impact of hormonal agent therapy on UI or concerning UI as a whole, contact our team to talk with a medical concierge.What is the most effective medicine for incontinence?
THERAPY OF DESIRE URINARY INCONTINENCE
The anticholinergic representatives oxybutynin (Ditropan; Oxytrol) and tolterodine (Detrol) are made use of extensively to treat urge urinary incontinence.
- This overview aims to demystify FEUCs, comparing them to traditional methods and highlighting what you need to take into consideration before choosing.
- The physical pressure of pregnancy and giving birth can occasionally cause medical therapies to fall short.
- Likewise referred to as chronic urinary retention; if you have this sort of urinary incontinence, you are unable to fully clear your bladder and may leak pee frequently.
- In addition, liquid management is crucial; females need to intend to drink sufficient water throughout the day while avoiding excessive intake before bedtime to minimize nighttime peeing.
- According to a study published in the Journal of American Urogynecologic Society, over 60% of grown-up females in the US deal with this unpleasant condition.
Social Links