September 6, 2024
The Effect Of Hormone Therapy On Urinary Incontinence Urinary Incontinence Institute
Effect Of Conjugated Estrogen In Tension Urinary System Incontinence In Ladies With Menopause Women due to the anatomy, social and social are much more prone to this illness [3] Urinary system incontinence is the uncontrolled loss of urine which is fairly demonstrable and is a social and health issue [4] The urinary incontinence that takes place in different kinds, including the serious kind of daily attacks a lot, an average of 1 to several times a week in the perspiration, the minor i.e. drop exuding once a week or month-to-month. Stress Urinary System Incontinence is a common trouble that in ladies its occurrence is 10% to 58.4% and most just recently, with increasing survival, its occurrence has actually enhanced [5] Women with severe intrinsic sphincter deficiency do not always have the usual urethral hypermobility during a Valsalva maneuver. This results in supposed lead pipeline urethra, where the urethra remains open at remainder.Understanding The Link Between Reduced Estrogen Degrees And Urinary Incontinence
Nonetheless, other root causes of urinary incontinence are long-term and related to problems that are handled throughout your life. If you have a persistent problem like diabetes mellitus or several sclerosis, you might have urinary incontinence for a. extended period of time. In those cases, it is necessary to talk with your company concerning the most effective means to manage your urinary incontinence to make sure that it does not hinder your life. Some ladies that undertake hormonal agent substitute treatment to deal with signs and symptoms of menopause experience urinary system incontinence. With this therapy, estrogen and progestin are added to the blood stream since the hormones are not being made by the body. As a negative effects of the drug, some ladies experience enhanced incontinence in the initial few days or weeks of the treatment and can make use of adult diapers to take care of the leakage. Bladder control issues occasionally continue even after making way of life modifications and trying bladder training. When various other choices don't function, it might be time to talk to your healthcare company regarding drugs. Urinary urinary incontinence can substantially influence your quality of life, but you don't need to live with it. Keeping hormonal balance during and after menopause aids improve the health and wellness and feature of your urinary system, and it could be the remedy you've been searching for. Within your urinary tract, estrogen assists maintain the cells healthy and adaptable, promoting ideal function of both your bladder and urethra.What hormonal agent stops pee?
earn less pee at night. Takeaway: If progesterone degrees are rising during and after your cycle, and progesterone creates your bladder to get much more often, it might cause urinary incontinence. Menstruation modifications. There are several factors your regular monthly period can transform, yet hormonal imbalance frequently plays a role.Hair concerns.
Exactly How To Take Care Of Urinary Incontinence And Low Estrogen
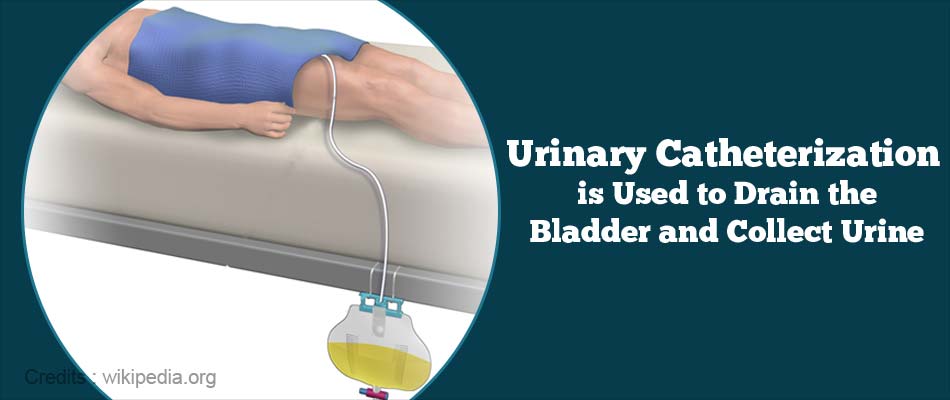
Urinary system incontinence might happen by itself or might be accompanied by various other obscure neurological signs and symptoms. Spine sores can modify understanding and parasympathetic tone, leading to urinary incontinence. Peripheral nerve illness such as diabetic peripheral neuropathy can trigger urinary system incontinence with a contractile disorder of the bladder. The cost of treating urinary incontinence in USA alone is $16.3 billion, 75% of which is invested in therapy of females. Urinary urinary incontinence can cause extended healthcare facility admission, urinary system tract infections, get in touch with dermatitis, and drops. Urinary system urinary incontinence is a leading cause of admission to an assisted living home when family members locate it as well hard to care for a family member with urinary incontinence.- Urinary incontinence is a loss of bladder control that's commonly seen in older grownups and women that have actually given birth or undergone menopause.
- Bladder control for ladies begins along with their final menstruation duration and boosts thereafter.
- As the womb increases the size of to suit the growing fetus, it exerts raising pressure on the bladder and pelvic flooring.
Social Links