
September 12, 2024
Whats The Treatment For Urinary Incontinence In Ladies?
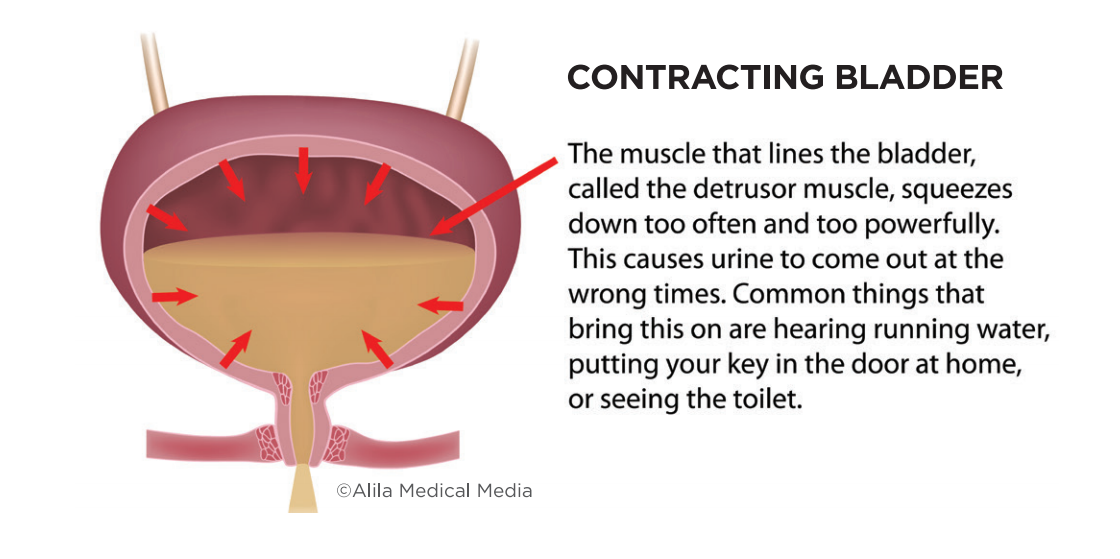
Urinary Incontinence Bladder function tests In Females Progesterone is a hormone launched by your ovaries throughout your menstruation. Its main feature is to prepare your body for maternity in instance an egg is fed throughout ovulation. If it is unlikely the symptoms belong to menopause, a medical professional may perform various other examinations to dismiss various other conditions, such as UTIs. They might also examine somebody's hormone degrees, bladder feature, or nerve function. If other non-invasive therapy options have stopped working to treat your urinary incontinence, there are a number of treatments that your provider could recommend.What Are The Types Of Urinary Incontinence?
What hormone maintains you from peeing?

Mayo Facility Press
For people with urinary system incontinence, it is necessary to seek advice from a health care service provider. In most cases, patients will certainly then be described an urogynecologist or urologist, a doctor who focuses on conditions of the urinary system system. Urinary system incontinence is diagnosed with a complete physical exam that focuses on the urinary system and nerves, reproductive body organs, and pee examples. Scientific research study and customer testimonials vouch for the transformative results attained with INNOVO.- Peripheral nerve disease such as diabetic person peripheral neuropathy can cause urinary system incontinence through a contractile dysfunction of the bladder.
- Speak with your doctor regarding these home therapy options for urinary incontinence prior to beginning any of them.
- As a result of the setting and feature of steroids in the urinary tract, using changed hormonal agent therapy in menopause has long attracted the interest of researchers and suppliers of health care in this area.
- Urinary urinary incontinence (UI) is likewise called "loss of bladder control" or "spontaneous urinary system leakage." Countless females experience it, and the frequency of UI often tends to boost as you get older.
- Your health care supplier might suggest that you revolve the place of your spot.
- Hormonal agent substitute therapies can-- often involving replacing estrogen that's reduced throughout menopause-- might likewise help recover regular bladder feature.
Social Links