September 13, 2024
Services For Your Urinary Incontinence: Melissa Grier, Md: Obgyn
Urinary Incontinence In Females: Kinds, Therapies, And Expectation The International Continence Society (ICS) standards advise starting with conventional therapies, including physical rehabilitation, pharmacotherapy, and behavior modification, to resolve urinary system incontinence. Difficulties might include anything from a boost in UTIs to growth of a microbial skin infection called cellulitis. Individuals going through therapy for urinary incontinence may also experience medication side effects such as dry mouth, irregular bowel movements, and high blood pressure.
Handling Menopause Incontinence In The House
Your hormonal agents (estrogen particularly) adjustment during menopause and this can change your bladder control. Minimally invasive treatments, such as genital pessaries and acupuncture, provide different services for handling incontinence without the need for significant surgical procedure. Genital pessaries are gadgets put into the vagina to provide support to the bladder and urethra, aiding to reduce leakage.
Find A Treatment Facility
Mirabegron has the potential to intensify hypertension131, yet is otherwise well tolerated compared with a lot of anticholinergics, with great persistence141. Mirabegron is best used in individuals for whom there is a contraindication to, or risk of cognitive or various other negative results from, anticholinergics. As your womb stretches to hold the expanding infant, a couple of things take place. Your bladder can be crushed by the expanding baby, making your bladder hold much less than before. Just do this until you discover how to find the muscular tissues-- stopping the circulation of urine mid-stream isn't healthy and balanced over an extended period of time. Urinary system urinary incontinence is a common condition influencing several people, especially postmenopausal females. Hormonal agent replacement treatment can aid alleviate this condition, primarily via estrogen supplements to help revive the vigor of your reproductive tract. However, this treatment has numerous dangers, and you should just do it after speaking with your doctor to understand what is ideal for your distinct case. If you have added inquiries concerning the influence of hormone treatment on UI or about UI generally, contact our team to talk with a medical attendant.
Estrogen Deficiency And Bladder Function
What vitamin quits over active bladder?
Vitamin D supplementation may be acquiring recognition as an effective method for prevention or relief of bladder signs such as over active bladder and urinary incontinence.
The ureters attach to the bladder, where the pee will certainly accumulate until it's time to leave the body. Your bladder is like a storage tank-- once the bladder is full, the brain sends out a signal that it's time to pee. Urine after that leaves the bladder when a muscular tissue opens up (sphincter), allowing the pee to move easily out of the body through the urethra. If urge urinary incontinence is the result of your detrusor muscle mass getting too often, sacral nerve excitement, likewise called sacral neuromodulation, may be recommended. It's taken into consideration for individuals that can not be helped by other types of therapy. When the infection is removed, your UI will likely solve or improve. When your bladder does not empty fully, this type of UI can reveal as constant urine dribbling. You can have a weak urinary stream, feel like peing at night (nocturia), and enhanced urinary hesitancy.
https://ewr1.vultrobjects.com/health-education/public-health/urethra/elders-and-maturing-bladder-control-problems.html Still, lots of people that struggle with urinary incontinence hesitate to resolve the concern due to the social stigma and fear connected to the subject. Individuals with incontinence ought to recognize that they are not the only one and need to be encouraged to get aid.
- This need to enhance the way signals are sent between your brain and your detrusor muscles and reduce your urges to pee.
- In parous ladies, vaginal distribution is a key flexible danger factor for grown-up tension urinary system incontinence, with stressful distribution uncovering incontinence in predisposed women177.
- Pastors representing numerous faiths are available all the time to supply assistance, convenience and guidance to people, family members and caregivers.
- For more information regarding urinary system incontinence or to get the care you need, call our office or timetable a consultation with Dr. Grier through our on the internet reservation feature.
- Estrogen is a substantial factor in maintaining the lining of the urethra and bladder strong and healthy.
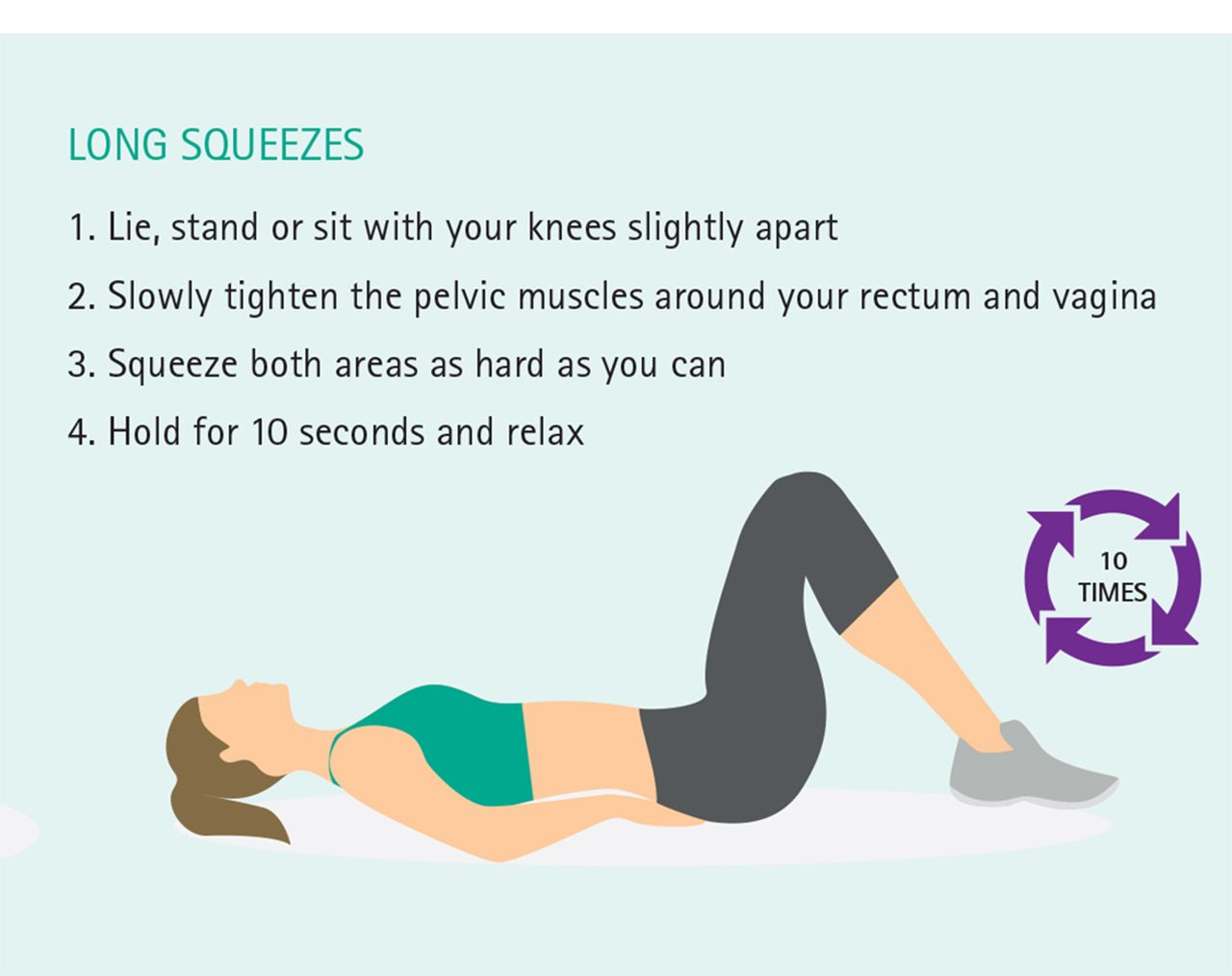
For the majority of women, home therapy or clinical therapy can treat or considerably improve urinary system incontinence. Likewise called chronic urinary retention; if you have this kind of urinary system incontinence, you are not able to totally clear your bladder and might leak urine often. This usually begins with straightforward measures, such as making use of vaginal oestrogen and seeing a physio therapist to help with pelvic flooring recovery. Understanding just how to re-train your bladder to hold bigger quantities of urine can help in reducing need to pass urine. Your physician may suggest surgical treatment if various other therapies have not helped. You might be referred to an expert urogynaecologist to talk about the advantages and risks of surgery for SUI. As a result of this, we are sensitive to your situation and deal with every one of our clients with miraculous regard and concern for discretion. According to a research released in the Journal of American Urogynecologic Culture, over 60% of grown-up women in the United States suffer from this awkward problem. It is known as urinary system incontinence (UI) and is an usual postmenopausal disorder. A few of its other risk factors consist of maternity and several genital births. Ladies with blended urinary incontinence experience signs and symptoms of both desire urinary incontinence and tension urinary incontinence. Pelvic floor muscle therapy is a vital part in managing menopause-related urinary incontinence, as it concentrates on strengthening the muscular tissues that support the bladder and urethra. This treatment not just enhances bladder control however also improves sex-related function and pelvic security. Normal interaction in pelvic flooring exercises can lead to significant improvements in signs and general quality of life for females experiencing incontinence. Way of living and behavior changes are important for taking care of menopause-related urinary incontinence. Also if you don't have incontinence, you should do pelvic flooring workouts to aid keep your pelvic area solid and continent. You can work with a therapist to better recognize how your body jobs. In biofeedback, a cable is connected to an electric patch over your bladder and urethral muscular tissues. It sends signals to a monitor, which notifies you when your muscular tissues are getting.