September 8, 2024
Impact Of Conjugated Estrogen In Stress And Anxiety Urinary Incontinence In Ladies With Menopause
Impact Of Conjugated Estrogen In Stress Urinary Incontinence In Females With Menopause Throughout a woman's life, from puberty to menopause, the fragile balance of hormonal agents coordinates a symphony of changes that can impact urinary system continence and pelvic floor toughness. In some cases, there are adjustments to your everyday life that can actually assist your urinary incontinence. These modifications commonly consist of exercises you can do to reinforce your pelvic floor muscular tissues, changes to your normal habits and an enhanced diet plan. Some people observe improvements by making these changes in your home and do not need added therapy. Hormone therapy (estrogen) in postmenopausal ladies alleviates urinary system frequency and dysuria and blood Pelvic Pain Relief flow of bladder cells rises and brings about raise the strength of muscle mass around the urethra [44] Steroid hormones along with ecological results in the urinary system tract have a central role in the neural control of peeing procedure. Nonetheless, the specific device of this action is unidentified, yet the presence of both sorts of estrogen receptors in the mind cortex, limbic system, the hippocampus and the brain has been verified [36]Comprehending The Web Link Between Reduced Estrogen Degrees And Urinary System Incontinence
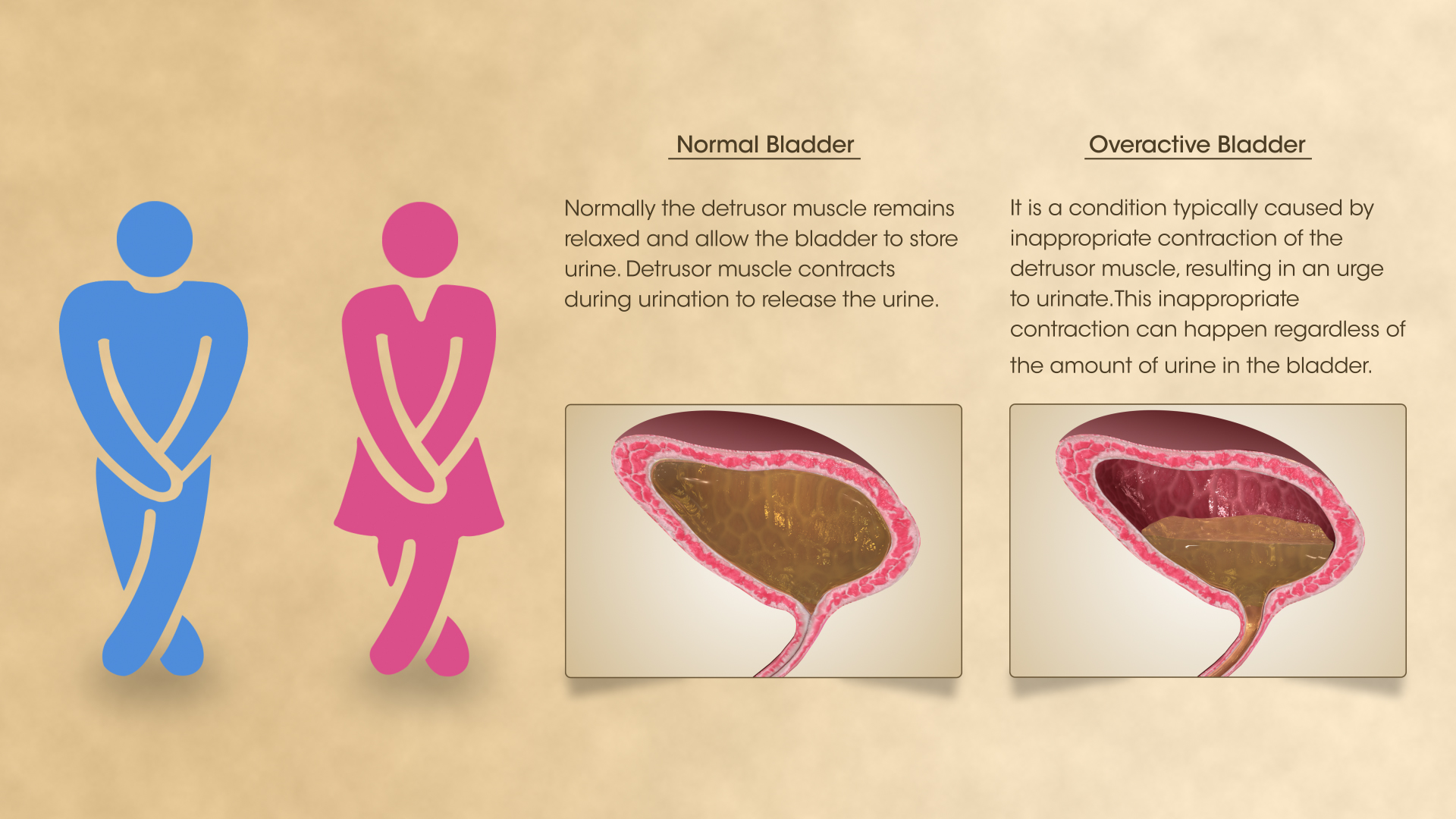
These hormone shifts can affect bladder feature and urinary system practices, materializing as urinary signs such as increased frequency, seriousness, or leak. Reduced levels of estrogen and urinary system incontinence go hand in hand. As ladies age and begin coming close to menopause, the ovaries reduce the process of making estrogen, and the levels of this women sex hormone naturally decrease in the body. [newline] Ultimately, with menopause, the manufacturing of estrogen stops, and this affects the body in several ways. Without estrogen, ladies locate it tough to preserve healthy and balanced urologic features during and after menopause. Bladder control for females begins together with their final menstruation duration and raises afterwards.How Is Incontinence Treated?
These medicines all have the potential to cause restlessness, tachycardia and high blood pressure. Ephedrine is provided at a dosage of 4 mg/kg every 8 to 12 hours. Numerous big type dogs might be begun on 25 mg every 8 hours, enhancing the dose to 50 mg if there is no clinical feedback at the lower dose. Phenylpropanolamine has the same potency and pharmacologic homes as ephedrine yet appears to cause less main nervous system stimulation. The suggested dose is 1.5 to 2.0 mg/kg twice daily to three times daily. Pseudoephedrine is similar to ephedrine and phenylpropanolamine.Understanding Stress And Anxiety Urinary Incontinence (sui)
Severe side effects from imipramine are unusual but can include heart and blood vessel problems. They might include an uneven heart beat and dizziness or fainting from reduced blood pressure when you stand quickly. Youngsters and older grownups may be particularly in danger of these side effects. Give your health care supplier a complete listing of your drugs prior to you begin taking this medicine.- The psychosocial prices and morbidities are much more tough to measure.
- Your healthcare supplier may recommend duplicating the shots once or twice a year.
- The maximal storage capacity of the bladder is gotten to, usually without the private understanding that this has actually taken place.
- If other techniques for assisting anxiety urinary incontinence don't function, your doctor could suggest surgical procedure.
- The most common genetic disorders creating urinary incontinence include ectopic ureter( s), and associated anatomic anomalies (license urachus, pseudohermaphrodites, and urethrorectal fistulae).
Just how can bladder leakage be stopped?
and structure.Skin problems.Sex-related symptoms.Weight changes.Mood and sleep issues.Digestive distress. Using low-dose, topical estrogen may assist. The medication comes in the kind of a genital cream, ring or patch. The estrogen might assist restore the tissues in the vaginal canal and urinary tract to eliminate some signs and symptoms. Topical estrogen could not be secure for people with a background of breast cancer cells, uterine cancer cells or both. Summary. Bladder disorder is a common obstacle, specifically later in life and throughout times of major hormone modification. Low estrogen bladder symptoms can include urinary incontinence, overactive bladder, and pain.
Social Links