September 1, 2024
Dealing With Urinary Incontinence: Social And Emotional Obstacles
Dealing Techniques For Women With Urinary Incontinence Some drugs, such as diuretics (" water tablets"), sedatives, sleeping pills, and some medications to treat anxiety can trigger incontinence or make it worse. Ask your medical professional if your urinary incontinence might be a side effect of your medicine and whether there are various other therapy choices for you. In contrast to our predictions, the direct effect of UI-related strategies was not observed on SF. One possible description might be that QoL is a broader construct, being easier to be impacted by concealing/ defensive actions to take care of UI. An additional description could be as a result of the reality that there are differences in between sexually and non-sexually energetic females, relating to the use of UI-strategies on Sexual Function.- Overactive bladder clients have a tendency to void in tiny quantities often throughout the entire period.
- It can be stressful going to function when you have urinary incontinence, specifically if you stress a lot about it while you exist.
- Clinical comorbidities, particularly conditions such as diabetic issues, ischaemic cardiovascular disease or congestive heart failure, neurological problems, persistent lung illness and weight problems, can intensify OAB and SUI symptoms.
- For women with MUI, practically one in five had moderate to serious levels of depression specified by a GDS score of 10 or even more and 30.0% had high degrees of anxiety defined by a PSS-4 score of 9 or even more.
- Detrusor overactivity, according to this concept, happens because of the premature shooting of stretch receptors in the bladder base second to poor endopelvic connective tissue support to the loading bladder.
What Is It Like Living With Urinary System Incontinence?
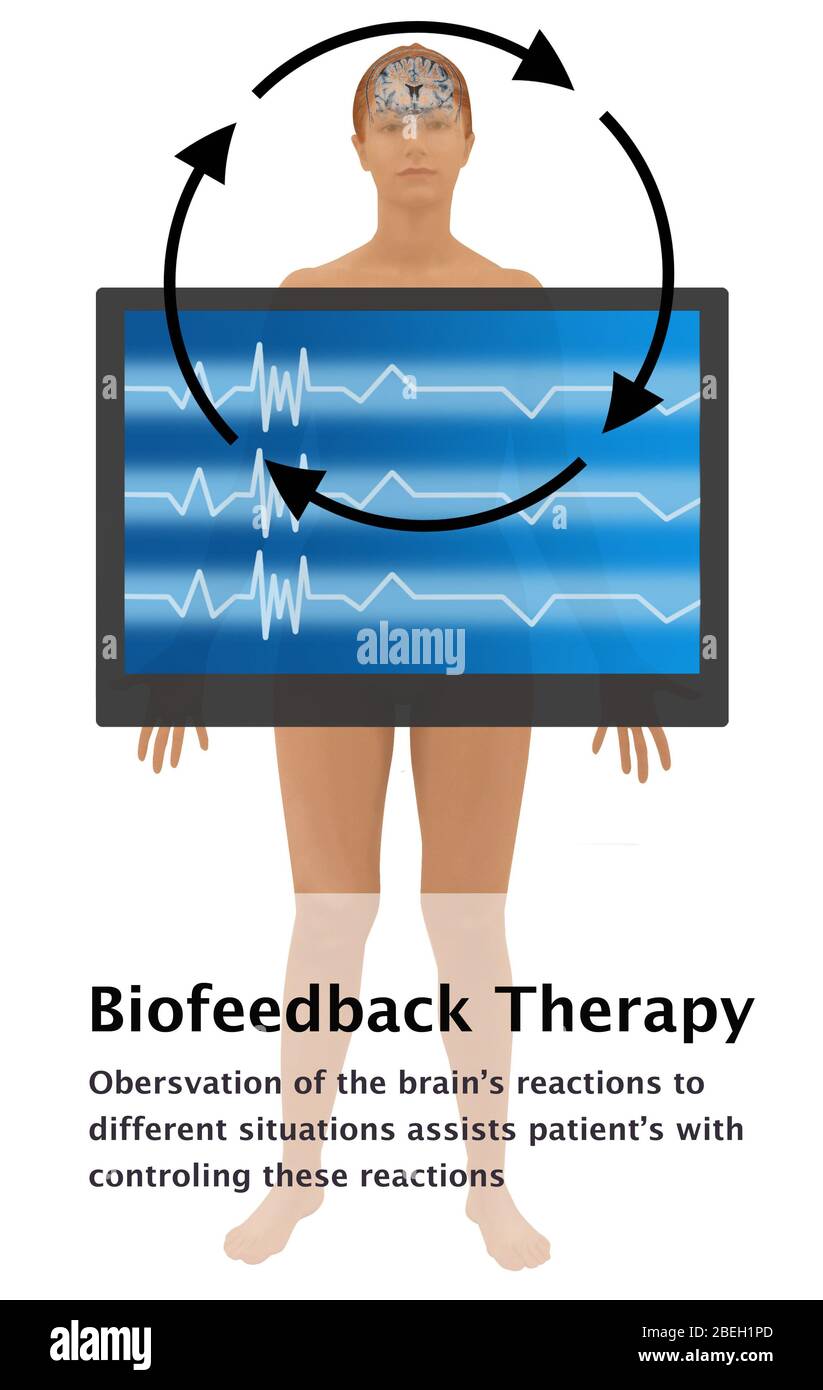
Preliminary administration of male urinary system incontinence usually consists of standard diagnostic examinations to omit any reversible conditions, such as a UTI (Number 1). Conservative, non-invasive treatment alternatives consist of lifestyle interventions, pelvic floor muscular tissue training (PFMT) with or without biofeedback, and bladder retraining.9 Way of life interventions consist of high levels of caffeine decrease, weight loss and cessation of smoking cigarettes. In some clients with co-existing urinary system signs and symptoms that are symptomatic of combined urinary incontinence, making use of an antimuscarinic medication might work to eliminate prospective detrusor overactivity.Individuals & Visitors
How to quit fretting about incontinence?
Vaginal mesh surgical treatment for stress incontinence is often called


tape surgical treatment. The mesh remains in the body completely. You'll be asleep during the procedure. It's often done as day surgical treatment, so you do not require to stay in hospital. Both physical and psychological stress and anxiety can contribute to SUI, which is
Continual Incontinence
Individuals with a neurogenic problem such as myelomeningocele may have an open bladder neck that causes serious intrinsic sphincter shortage and urinary loss. Multiple sclerosis should be considered in any kind of person without proof of urinary system infection who has anecdotal or fast start of urinary system signs. Urinary urinary incontinence might take place by itself or might be gone along with by other vague neurological signs and symptoms. Spine sores can alter sympathetic and parasympathetic tone, leading to urinary system incontinence. Urinary system urinary incontinence in end-of-life care can be testing to take care of and ought to be taken care of on a case-by-case basis. In some instances, an indwelling catheter or prophylactic catheter might be used to make best use of patient comfort during the last phases of life. An extensive individual history ought to assist the clinician towards an ideal physical exam. Surgical history ought to likewise be evaluated as the makeup and innervation entailed might have been influenced by previous surgeries. Male stress and anxiety urinary incontinence, for example, is almost always because of postoperative difficulties from urologic surgical procedure. Please see StatPearls' friend source, "Slings for Male Incontinence," for further details. If it's not dealt with, CES could result in long-term never ever damage or even paralysis. An uncommon disorder called cauda equina disorder (CES) can create both back pain and incontinence. It happens when a package of nerves in your reduced spinal column (the cauda equina) obtain squeezed or compressed. Due to the fact that these nerves aid supply feeling and movement to your legs and groin area, CES can result in urinary system or digestive tract urinary incontinence as well as pain in the back. Individuals that experience a frequent, immediate demand to urinate or have pee leak ought to review treatment alternatives with a physician. The physician can provide a medical diagnosis and assembled a therapy strategy. Pelvic floor workouts can aid restrengthen these muscle mass and improve the signs and symptoms of urinary incontinence and OAB. A physical therapist can work with a specific to come up with a workout plan that benefits them. Without reliable treatment, urinary system incontinence can have a negative outcome. Long term contact of pee with the vulnerable skin creates call dermatitis and skin failure. If left unattended, these skin problems may cause push sores and abscess, possibly resulting in additional infections.Social Links